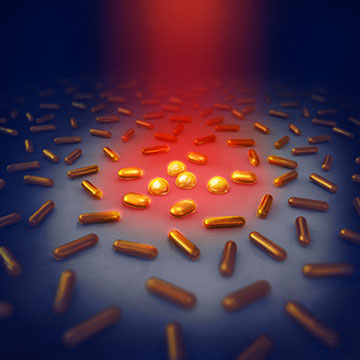
The illustration shows how the gold nanorods heat up when illuminated with NIR light. At temperatures above 120°C , the gold rods begin to change shape, and their optical properties change. [Image: Daniel Spacek, Neuron Collective, neuroncollective.com]
The unique characteristics of gold nanoparticles, such as tunable optical properties and localized heat emission, make them suitable for numerous biomedical applications. In particular, photothermal therapy (PTT) uses the heat released from gold nanoparticles upon excitation with resonant light to kill tumor cells.
Now, researchers in Sweden have evaluated the photothermal properties of gold nanorods to explore their potential as antibacterial agents (Nano Lett., doi: 10.1002/nano.202100255). The approach, which shows promise for sterilizing medical implants, is the first demonstration of PTT with gold nanorods to create an antibacterial surface.
Frying bacteria to death
In traditional PTT for cancer treatment, gold nanorods bound to tumor cells absorb light in the near-infrared (NIR) range and then convert the photon energy to heat. The increase in temperature of the tumor’s microenvironment induces apoptosis or necrosis of the tumor cells.
Martin Andersson, Chalmers University of Technology, and his lab wanted to investigate a different clinical application for PTT with gold nanorods. Surgical procedures that involve foreign materials, such as hip and knee prostheses, carry a risk of infection. Infection prevention is a critical component of joint replacement surgery, since it is difficult for the immune system to attack bacteria on the surface of metal or plastic implants.
Andersson and his colleagues proposed a technology that would attach gold nanorods to the implant surface and implement PTT to kill any lingering bacteria. In the current study, they sought to better understand the effect of nanoparticle shape and collective heating on PTT antibacterial performance.
“The gold rods absorb the light, the electrons in the gold are set in motion and finally the nanorods emit heat,” said study author Maja Uusitalo in a press release accompanying the research. “You could say that the gold nanorods work like small frying pans that fry the bacteria to death.”
Temperature parameters
Andersson and his colleagues proposed a technology that would attach gold nanorods to the implant surface and implement PTT to kill any lingering bacteria.
The researchers synthesized two populations of gold nanorods with different aspect ratios and electrostatically immobilized them onto glass substrates. They investigated collective heating effects by adjusting the surface coverage of gold nanorods and using X-ray diffraction to determine their exact temperature as well as any structural changes.
“The temperature must not exceed 120°C, as higher temperatures cause the nanorods to lose their shape and transform into spheres,” said Uusitalo. “As a result, they lose their optical properties and can no longer absorb NIR light effectively, which prevents the rods from heating up.”
Up until that point of maximum heat, the results show a linear temperature increase with laser power, aligning with theoretical predictions, and a slope dependent on the coverage of gold nanorods on the surface. Heating is very local, with low energy transfer to surrounding tissue.
“We can control when the surface should be antibacterial and when it should not. When we turn off the light, the surface is no longer antibacterial and reverts to its original state,” said Andersson. “This is an advantage because many antibacterial surfaces usually have negative effects on healing.”
