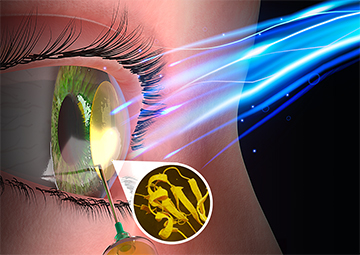
Researchers in Canada showed that an injectable biomaterial activated by pulses of low-energy blue light has potential for on-the-spot repair of corneas. [Image: Faculty of Medicine, University of Ottawa]
Scientists are racing to develop alternatives to human donor corneas to make up for the shortage of donated tissues worldwide. Despite these efforts, corneal transplant continues to be the gold-standard treatment for diseases that thin the outer layer of the eyeball.
In the latest study, researchers in Canada have developed biomaterials that can be injected directly into the damaged area of the eye (Adv. Funct. Mater., doi: 10.1002/adfm.202302721). When activated with pulses of low-energy blue light, the materials harden to form a structure that reshapes and thickens the injured tissue.
“Our technology is a leap in the field of corneal repair,” said Emilio Alarcon, medical professor and bioengineering researcher at University of Ottawa, in a press release accompanying the paper. “We are confident this could become a practical solution to treat patients living with diseases that negatively impact corneal shape and geometry.”
Low-dose pulsed blue light
The cornea provides about two-thirds of the eye’s focusing power, and diseases that lead to permanent loss of its transparency are among the most common causes of blindness, affecting 57 million people globally. While less dire, corneal thinning can also be problematic because it distorts one’s vision. A common cornea-thinning disease, keratoconus, affects 21 out of 1000 men and 18 out of 1000 women.
In their study, Alarcon and colleagues show that using injectable biomaterials composed of peptides and glycosaminoglycans could help reinforce corneas to promote healing, which would allow patients to avoid invasive transplants. The team’s proposed method is to inject the viscous liquid into a small, surgically created pocket in the tissue. Then the researchers illuminate the area for 10 minutes with 460-nm light to harden the liquid to form a tissue-like 3D structure. They suggested pulsing the light—turning it on for 2.5 s and then off for 2.5 s—at a low dosage of 8.5 mW/cm2 to avoid damaging the retina.

Emilio Alarcon [Image: Faculty of Medicine, University of Ottawa]
When the researchers tested their materials using pig corneas ex vivo, they found that the resulting transparent 3D structure had similar properties to the swine tissue. Optical coherence tomography imaging also revealed that the structure remained stable for 48 hours after the injection.
Alarcon and colleagues then turned to rats for in vivo experiments. They monitored the rats for up to six weeks and found that the thickened material was also stable in the rodents’ eyes and didn’t cause significant inflammation. Based on the results of his team’s experiments, “We anticipate our material will remain stable and be nontoxic in human corneas,” Alarcon said.
The road to human trials
Getting the research to the publication stage took the team seven years, according to the press release. “We had to engineer each part of the components involved in the technology, from the light source to the molecules used in the study,” Alarcon added. “The technology was developed to be clinically translatable, meaning all components must be designed to be ultimately manufacturable following strict standards for sterility.”
The results are being used for a patent application, which is currently under negotiations for licensing. Before human clinical trials can be conducted, experiments on large animal models will have to be carried out as well.
