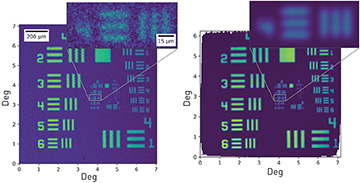
 Images of a 1951 USAF resolution target obtained with a single raster scan (left) and using our calibration technique (right). [Enlarge figure]
Images of a 1951 USAF resolution target obtained with a single raster scan (left) and using our calibration technique (right). [Enlarge figure]
Ophthalmic imaging science has made tremendous progress, spurred by new imaging techniques, increasing computational power and novel visualization technologies. Numerous instruments capable of showing the eye’s inner workings with exquisite detail have been developed.1
One of the most widely used instruments in clinical ophthalmology is the scanning laser ophthalmoscope (SLO). This instrument records the reflected intensity of a laser source swept across a target on a transverse plane; the resulting reflectivity map is then interpreted clinically in retinal or corneal diagnostics. Such diagnostics not only are useful in finding traditional ophthalmic pathologies, but are also becoming a powerful tool to detect the earliest signs of neurodegenerative diseases.2 Recent advances in SLO technology, including eye-motion compensation and concomitant fluorescence imaging, have improved the performance and usefulness of SLOs, which now constitute a workhorse of clinical ophthalmology.
A fundamental limitation of SLOs, however, is the precision with which the scanning laser’s position is known. Accurate knowledge of beam location is crucial for producing accurate, clinically significant maps. Yet state-of-the-art SLOs use electromechanical scanning mechanisms, which inherently introduce noise in the beam’s position. In addition, geometrical distortions of the scanning and signal-collecting optical systems add further uncertainty. The collective result is a deformed image.
Different efforts to tackle the problem have been reported with varying degrees of success. The most common approach has been to model the system’s optical distortions and then use the image of a calibrated target object to estimate the scanning trajectory. In recent work, we have solved the problem of localizing the coordinates of the scanning trajectory by measuring the actual position of each individual point in the trajectory.3
We achieve this measurement by using a collection of laterally displaced copies of the trajectory to image partial sections of our object of interest. We then find the distance between adjacent image pairs using their partial overlaps. In other words, we translate the problem of mapping a set of unknown coordinate points into a manifold of image-registration tasks, which are readily executed with high computational efficiency. We then use a multidimensional-scaling (MDS) algorithm, a powerful mathematical technique capable of generating an accurate map of spatial points from the known distances between them.4
Using our calibration protocol, we have been able to produce images with a spatial resolution higher than the diffraction limit of the scanning optical system, without the need for a calibrated target. Moreover, because we use multiple measurements to find the beam position, uncorrelated noise sources are largely suppressed from our images.
Calibrating beam trajectories with this level of detail opens new and exciting avenues for clinical applications of SLOs. We are now focusing on integration of ophthalmic SLOs with diverse, parallel multimodal imaging, to aid the search for the earliest known biomarkers of neurodegeneration.
Researchers
M. Meina, P. Stremplewski, C. López-Mariscal, S. Tamborski, M.M. Bartuzel and M. Szkulmowski, Nicolaus Copernicus University in Toruń, Toruń, Poland
References
1. M. Bartuzel et al. Biomed. Opt. Express 11, 3164 (2020).
2. R. Rodríguez-Labrada et al., I. Mravicic, Ed., in Eye Motility (IntechOpen, 2019).
3. M. Meina et al. Opt. Lett. 46, 5377 (2021).
4. G.T.F. de Abreu and G. Destino, 2007 IEEE Wirel. Commun. Netw. Conf., pp. 4430–4434 (2007).

