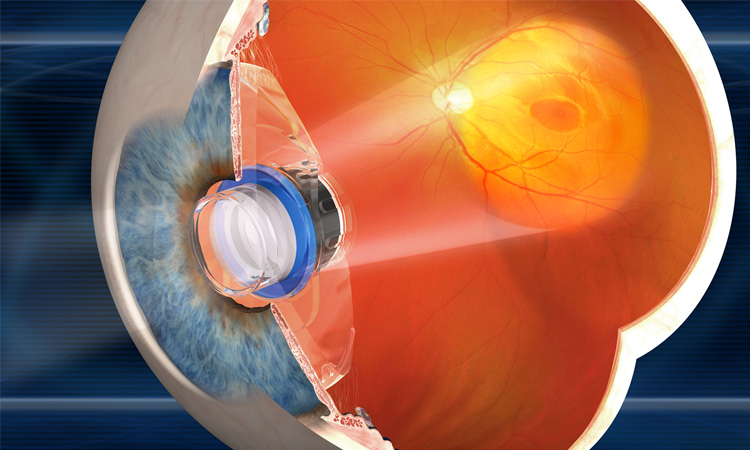
 An implantable miniature telescope from the company VisionCare focuses a magnified view of intact central vision onto a healthy part of the macula, to address age-related macular degeneration. [VisionCare]
An implantable miniature telescope from the company VisionCare focuses a magnified view of intact central vision onto a healthy part of the macula, to address age-related macular degeneration. [VisionCare]
Ophthalmology has made incredible strides in the past decade in surgical vision correction and disease diagnosis—yet those facing complete blindness have remained largely without hope. Now, however, scientists and surgeons have begun accomplishing the seemingly impossible: restoring sight to those who had lost it.
After 25 years of development, optics and optoelectronic technology in the form of bionic eye implants have emerged as a promising approach to sight restoration. In just the past year, bionic vision prosthetics have progressed from proving their efficacy in clinical trials to becoming a commercial reality. As of early 2017, the prosthetic eye is already providing life-changing sight to nearly 900 severely vision-impaired patients around the world.
According to the World Health Organization, over 285 million people worldwide are blind or vision impaired—90 percent of them living in low-income settings, and 82 percent at least 50 years of age. Loss of vision means inability to read, identify loved ones and confidently execute everyday activities like walking down the street or reaching for a glass of water.
Scientists and surgeons have begun accomplishing the seemingly impossible: restoring sight to those who had lost it.
Among the most common causes of blindness worldwide are age-related diseases such cataracts, age-related macular degeneration (AMD), diabetic retinopathy and glaucoma. Cataracts, the most common visual impairment globally, affect as many as 24.4 million people in the United States alone as of 2010, a number expected to double by 2050.
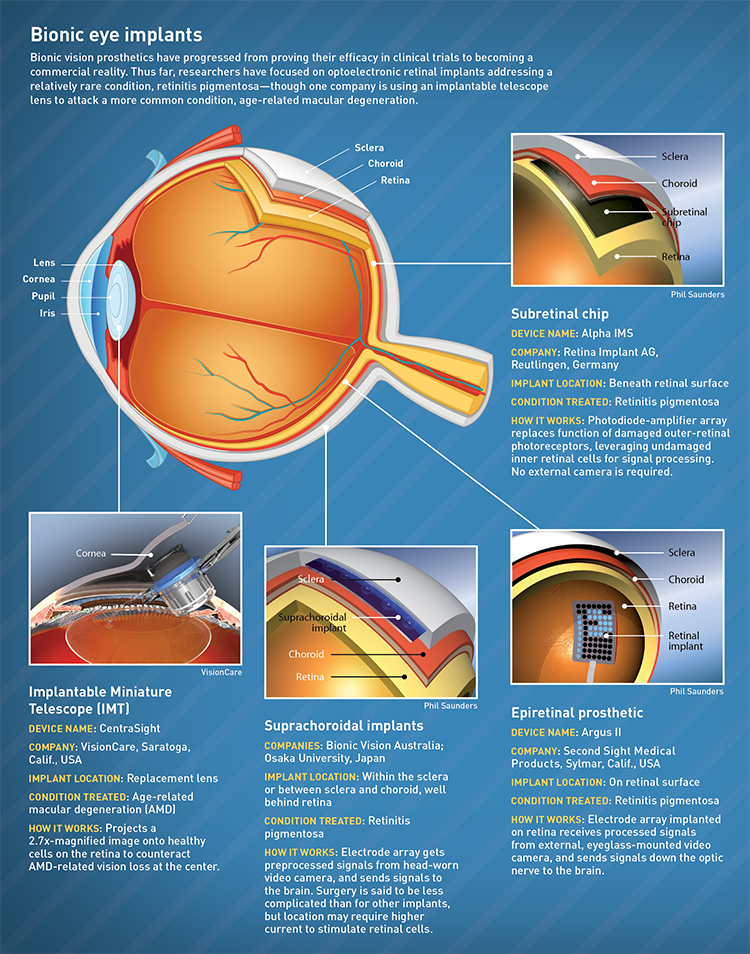
Globally, cataracts are commonly treated with surgery to replace the clouded lens of the eye with a synthetic intraocular lens (IOL). But treatment for other, more complicated conditions has remained elusive. AMD—estimated to affect 11 million people in the United States alone and to cause blindness in 2 million—arises from decay in the retinal pigment epithelium layer in the back of the eye; the decay forms a “grayed-out” blind spot in the middle of the visual field that grows over time. So-called wet AMD, characterized by abnormal bleeding under the macula, can be treated with injections inside the eye. But dry AMD has no treatment.
The first commercial retinal implant
To attack these more complex conditions, academic and commercial entities are hot on the trail of practical prosthetics that work in lieu of a damaged or diseased eye. The idea of using electrical current to simulate photons in the eyes of the blind has actually been around for centuries. In many cases of blindness, the light is blocked or not detected by diseased or damaged retinal cells. However, if some cells of the inner eye and the optic nerve have enough function and if the visual cortex operates normally, vision processing abilities remain. This is where vision implants shine.
For this reason, one of the first diseases targeted with eye implants has been not AMD, but a much rarer condition: retinitis pigmentosa (RP), which affects approximately 100,000 people in the United States. A progressively degenerative disease, RP is an inheritable condition in which rods and cones—the eye’s photoreceptor and color cells—die over time, causing vision to dim from periphery to center. The tunnel vision of RP is the opposite of AMD, which dims from the center out. Both can progress into crippling blindness with no cure; RP can lead to complete blindness in a matter of years.
 (Top) Argus II ambassador Fran Fulton with surgeon Allen Ho of the Wills Eye Institute. (Bottom) Argus II ambassador Terry Byland identifies a white line on the floor, a simple but profound feat that enables mobility and independence in the blind. [Second Sight Medical Products]
(Top) Argus II ambassador Fran Fulton with surgeon Allen Ho of the Wills Eye Institute. (Bottom) Argus II ambassador Terry Byland identifies a white line on the floor, a simple but profound feat that enables mobility and independence in the blind. [Second Sight Medical Products]
The first commercially available artificial retina system to treat RP is the Argus II, manufactured by Second Sight Medical Products in Sylmar, Calif., USA. The Argus, an epiretinal system (that is, one placed on the top of the retinal surface), was first implanted in a human patient in 2006. More patient implants followed, and after years of clinical trials, training of patients, development of new measurement techniques, long-term safety studies and device development, the Argus II received the first European Conformity (CE) Mark of approval for a wireless retinal implant in Europe in 2011, and the U.S. Food and Drug Administration (FDA) Humanitarian Device Exemption in 2013. In 2014, Second Sight commercially launched the implant in the United States for treating RP in adults. Today, it is the only artificial retina commercially available in the country.
The Argus II implant works via a tiny array of 60 electrodes tacked to the retina in the back of the eye. The user wears a small video camera and transmitter mounted on a pair of eyeglasses, which wirelessly transmits processed signals to the electrode array. The electrodes bypass the damaged retina and send signals directly down the optic nerve to the brain, which interprets them as visual images.
The outpatient surgery takes around three hours. In three weeks, the patient can wear the glasses. The sight restored to the RP sufferers doesn’t approach the “cyber vision” popularized by The Terminator or The Six Million Dollar Man; the resulting images are low-resolution lights that flicker in black and white, enabling users to see walls, lights and facial outlines. Yet restoring even the smallest amount of sight to someone diagnosed with a lifetime of darkness can make a world of difference.
After 20 years of blindness caused by RP, Rozina Issani, 55, first saw light via the Argus II system, implanted by Dr. Robert Devenyi at Toronto Western Hospital, Canada, in March 2015. At the annual American Academy of Ophthalmology meeting in Chicago, USA, in October 2016, Issani and other patients described how the implant has affected them. “When I first put on the glasses and saw light, it brought tears to my eyes,” she said.
Patients require occupational training to enhance their use of the system, but with practice, the brain’s interpretation of the rough signal improves over time. Issani added, “I can see the trees now. I can see light poles, and where to press the button to change the light in the crosswalk. I can see the full moon.”
“When I turned on the glasses, it was an ‘Oh my God’ moment,” said Fran Fulton, who was implanted with the Argus II in July 2014 after 15 years of blindness. “I was able to spot things on the wall and see people come in the room. I was able to walk right through the doorframe. It’s hard to tell a garbage can from someone sitting on the sidewalk, but I can go around it. I can now make decisions and maintain my independence.”
More than 200 patients have received the Argus II implant for treatment of RP. “It’s taken 25 years to get an artificial retina commercially available in the USA, Europe and Canada. But it’s been worth it,” says Dr. Robert Greenberg, chairman of the board of directors of Second Sight. “It’s a pretty dramatic thing, taking people who are completely blind with RP and giving them sight.”
The company will continue to improve the implant by, for example, making updates downloadable via a patient’s cellphone, and enabling color detection and improved resolution. The process of obtaining approval in South America and Asia is underway.
Seeking resolution
Another retinal implant, the Alpha IMS from the German company Retina Implant AG, became, in 2013, the second wireless retinal implant to receive the CE mark in Europe. The device is a tiny microchip measuring 3 mm2 with 1,500 microphotodiode-amplifier pixels that replace photoreceptor function in the eye. In contrast to the epiretinal Argus II, the Alpha is a subretinal device, implanted beneath the damaged retina to harness the full signal-processing potential of the intact bipolar cells of the inner retina.
In early 2017, Retina Implant AG announced the results of clinical trials on patients with RP who were implanted with the Alpha IMS subretinal prosthesis. The studies showed improved vision and subjective improvement in daily activities. The Alpha device enables patients to use natural eye movements to track objects over a central visual field of 10 to 15 degrees, without the head-mounted camera required by the Argus device. The Alpha claims to have enabled visual acuity of up to 20/546, the highest published resolution for a neuroprosthetic visual implant yet.
A next-generation device from the company, the Alpha AMS, featuring 1,600 pixels, concluded clinical trials early this year. Results were positive; patients with severe blindness from RP achieved improved object detection and identification. Additional clinical trials of the Alpha AMS involving 16 patients will be completed by the end of 2017, with additional trials and studies planned in France and the United States.
 One of the first recipients of the prototype 24-channel wearable vision processor developed at Bionic Vision Australia, blind patient Dianne Ashworth, navigates a makeshift obstacle course at the Royal Victorian Eye and Ear Hospital in Melbourne, Australia, supervised by researchers Chris McCarthy and Fleur O’Hare. [David Nayagam/Bionics Institute]
One of the first recipients of the prototype 24-channel wearable vision processor developed at Bionic Vision Australia, blind patient Dianne Ashworth, navigates a makeshift obstacle course at the Royal Victorian Eye and Ear Hospital in Melbourne, Australia, supervised by researchers Chris McCarthy and Fleur O’Hare. [David Nayagam/Bionics Institute]
Supra-safe approach
Another surgical approach to retinal implants, about to begin a second set of clinical trials in Australia, is implantation between the sclera (the tough, white outer layer of the eyeball) and the choroid (the layer of blood vessels between the sclera and the retina). According to Anthony Burkitt, a neuroengineering professor at the University of Melbourne and director of the Bionic Vision Australia (BVA) research consortium, suprachoroidal implants may offer greater device stability than subretinal or epiretinal approaches, as well as increased patient safety, as the surgery is relatively straightforward and less invasive.
“We make an incision in the peripheral part of the sclera to create a pocket at the back of the eye, which is a safe, stable location to place the electrode array,” said Burkitt. “It stays quite happily there for the life of the implant.” Carla Abbott, of the Centre for Eye Research Australia in Melbourne, adds that suprachoroidal surgery does not breach the retinal tissue, nor does it require removal of the gel-like vitreous humor from inside the eye, both of which increase the risk for complications that can lead to poor visual outcomes such as retinal detachment or infection.
The prototype BVA device had 24 channels in a medical-grade silicon substrate measuring 8 x 19 mm. A cluster of 33 stimulating electrodes are situated in a hexagon, with an outer ring operating together and 20 stimulated individually. The pilot clinical trial involved implanting the device in three patients with profound vision loss from RP, who wore camera headgear with an image processing unit that sent the signal to the implant.
“The advantage of the camera, as opposed to using photodiodes to stimulate the back of the retina, is that we have control over the stimulation,” said Burkitt. The researchers can use advanced processing to help transform the image into the most useful form for the patient. And, continues Burkitt, “The patients became an amazing part of the research team. They came in one day a week for two years to help us learn how to control the stimulation and help them move around in their environment.”
One exciting discovery for the team was realizing that rather than processing the signal to make dark objects darker and light objects lighter, it was more helpful to encode objects according to what’s nearby, so the patients could better avoid tripping over things. The team’s “bit encoding” to make nearby objects brighter and far away objects darker is now a patented part of the BVA system.
 The suprachoroidal implant for retinitis pigmentosa places an array of stimulating electrodes behind the choroid (the layer of blood vessels between the sclera and the retina). [David Nayagam/Bioinics Institute]
The suprachoroidal implant for retinitis pigmentosa places an array of stimulating electrodes behind the choroid (the layer of blood vessels between the sclera and the retina). [David Nayagam/Bioinics Institute]
According to Burkitt, the patients felt the implants were beneficial, even in unexpected ways. “Sometimes they don’t know how far away someone has moved. This technology helped them discern whether they were still talking to a person in the room or talking to the houseplant. That’s a really important part of everyday living.” The next step for the Australian bionics team is a clinical trial of a 44-channel fully implantable suprachoroidal prosthesis, set to begin in 2017.
A research group in Japan is also pursuing a suprachoroidal prosthesis similar to that at BVI, with the implant located within the sclera. In May 2016, Takashi Fujikado, professor of applied visual science at Osaka University, and his team reported the results of clinical trials using a 49-channel suprachoroidal-transretinal stimulation (STS) retinal prosthesis in three patients with advanced RP. Their placement of the electrode array in the scleral pocket imparts greater stability than the epi- and subretinal approaches, like the Australian study, but requires higher current to stimulate the retina. Surprisingly, the side-effects of such implants may include neuro-enhancement resulting in improvement in a patient’s residual natural vision. The next-generation system employs a dual array to expand the visual field beyond the patients’ horizontal field of view in the initial STS device of 15.1 degrees.
More than 600 AMD patients have received another, very different type of implant for restoring vision: an implantable miniature telescope.
Beyond retinitis pigmentosa
Ironically, the drastic, total vision loss characteristic of RP patients makes it a better candidate for surgical implant research than a far more common cause of vision loss, AMD. “If we treat totally blind patients with RP, any detection of photons is an improvement,” says Second Sight’s Greenberg. “With macular degeneration, the patients often have remaining peripheral vision, so it’s harder to justify the expense and surgery. We can’t yet prove that the implant provides better results than their remaining peripheral vision.”
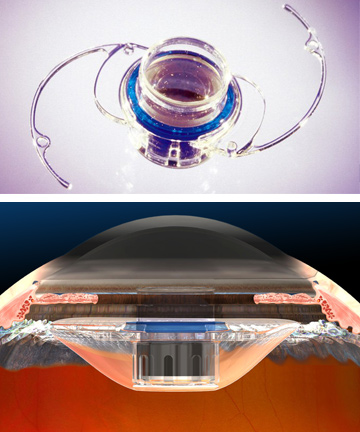 The implantable miniature telescope (IMT) from VisionCare, implanted in place of the lens of the eye, projects a 2.7x magnified image on the retina to treat blindness caused by age-related macular degeneration. The 1/8th-inch device is held in place behind the iris. [VisionCare]
The implantable miniature telescope (IMT) from VisionCare, implanted in place of the lens of the eye, projects a 2.7x magnified image on the retina to treat blindness caused by age-related macular degeneration. The 1/8th-inch device is held in place behind the iris. [VisionCare]
It’s thus exciting that more than 600 AMD patients have received another, very different type of implant for restoring vision: an implantable miniature telescope (IMT) from VisionCare, Inc. of Saratoga, Calif., USA. The pea-sized IMT is implanted behind the iris of one eye. The central vision missing due to retinal scarring is magnified 2.7 times by the telescope, and projected onto the healthy part of the retina around the scar. With practice, users learn to use that eye for central vision, and the other eye for peripheral vision. The projected image is magnified, typically leaving a small white spot in the center, but nonetheless offering a significant improvement over total central blindness. The average patient picks up three or more lines of vision on the standard eye chart, according to Blake Michaels, VisionCare’s CEO.
The IMT is the only FDA-approved implant for end-stage AMD. But so far, the device implantation has been limited to patients who have not previously had cataract surgery. This is problematic, says Michaels, because typical patients with end-stage AMD are in their 70s or 80s, an age by which many have already had routine cataract surgery to replace their clouded lens with a new IOL. In early 2017, VisionCare announced FDA approval for a clinical trial in post-cataract surgery patients. This study, which is currently enlisting patients, hopes to demonstrate that replacing an IOL with an IMT is feasible and safe.
On another front, in October 2016, Second Sight announced the first successful human implantation and activation of the Orion I, a wireless multichannel vision prosthesis that provides neurostimulation of the visual cortex. The system works like a cochlear implant, but goes into the surface of the brain near the visual cortex instead of the auditory cortex. If successful, Orion could in principle bypass any eye condition, to help all blind people, not just those afflicted with RP (the focus of the company’s Argus product). An initial proof-of-concept study, coupled with pre-clinical work gathered to date, will ready Second Sight to apply for FDA approval soon, and conduct an initial clinical trial of the complete Orion I system—including the camera and glasses.
Will brain-stem vision prosthetics become as common as cochlear implants? Cochlear implants took about 30 years to get from concept to market, according to Greenberg. “With the Argus system,” he says, “the challenge was to establish the level of vision improvement.” But no standards existed for measuring the restoration of vision in completely blind people.
“It hadn’t been done before,” said Greenberg. “We had to develop completely new techniques, working with the community and the FDA to test the patients and prove we could restore vision. We had to establish new objective tests and subjective ways to measure improvements in their daily life.” Now, the international vision-implant community has developed a multinational task force to establish measurement standards for vision restoration. With Orion, these new measurement standards will already be in place. Greenberg estimates the path from concept to patients will be relatively short—within the next few years.
Which of the techniques will succeed in the end? According to Burkitt, that’s difficult to predict; all current approaches involve surgery whose outcome varies by placement, and all produce comparable visual performance for patients. “We’re all trying to see how much benefit patients can get in the long term,” said Burkitt. “Competition is extremely good for the field, and it could well be that different conditions and types of vision loss require several different approaches.”
Valerie C. Coffey is a freelance science and technology writer and editor based in Palm Desert, Calif., USA.
References and Resources
-
L.N. Ayton et al. “First-in-human trial of a novel suprachoroidal retinal prosthesis,” PLoS ONE 9, 12 (2014).
-
J.F. Rizzo and L.N. Ayton. “Psychophysical testing of visual prosthetic devices: a call to establish a multi‐national joint task force,” J. Neural Eng. 11 (2014).
-
A. Brandli et al. “Progress in the clinical development and vision prostheses: an update,” Eye Brain 1, 15 (2016).
-
T. Fujikado et al. “One-year outcome of 49-channel suprachoroidal-transretinal stiumlation porsthesis in patients with advanced retinitis pigmentosa,” IOVS 57, 6147 (2016).
-
Z. Hafed et al. “Oculomotor behavior of blind patients seeing with a subretinal visual implant,” Vis. Res. 118, 119 (2016).
-
M. Humayun et al. “The bionic eye,” Ophthalmology 123, S89 (2016).
-
R.E. MacLaren. “Electronic retinal implant surgery,” Eye 31, 191 (2017).

