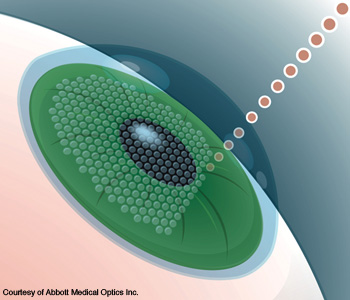
 Graphic illustration of femtosecond laser creating corneal flap during LASIK surgery.
Graphic illustration of femtosecond laser creating corneal flap during LASIK surgery.
Lasers have become as essential to the practicing ophthalmologist as the scalpel, the magnifier and sterile gloves. A beam of light can reshape a cornea to improve its focus, create a channel within the eye to relieve the intraocular pressure of glaucoma or cauterize tiny hemorrhages.
During the past decade, lasers have been branching out from ophthalmologic treatments into the diagnostic realm. Some of the hottest areas in vision research involve boosting laser-based microscopic techniques with adaptive optics to enable physicians to detect glaucoma and other devastating eye diseases in their earliest stages. Since the retina is the only part of the central nervous system that physicians can see without having to perform surgery, eye imaging with laser light could even give neurologists a non-invasive view into Alzheimer’s disease in its early stages.
Retinal fluorescence and disease diagnosis
Thanks to a combination of scanning laser ophthalmoscopy and computer processing, scientists can study naturally occurring retinal fluorescence, which could serve as an early-warning marker of glaucoma, macular degeneration and other eyesight-stealing diseases.
Before those technologies existed, researchers could not detect this autofluorescence, which comes from a pigment called lipofuscin, in the living eye. Lipofuscin is made up of yellow-brown granules and accumulates in various parts of the human body—including the retina—as part of the “wear and tear” of aging at the cellular level. An abnormal amount of this buildup in the retinal ganglion cells and retinal pigment epithelium has been implicated in age-related macular degeneration, a disorder of the macula of the eye that makes it difficult for people to see fine details. The macula is the portion of the retina that is responsible for central vision.
At first, scientists knew about the existence of the fluorescence from lipofuscin only from post-mortem studies because the signal was too low in living subjects, said Frederick W. Fitzke, professor of visual optics and psychophysics at University College London (UCL)’s Institute of Ophthalmology (U.K.). The fluorescence occurs under 488-nm light from an argon laser, and the confocal imaging technology excludes the fluorescence from the eye’s crystalline lens, which would otherwise mask the target signal from the retina.
The confocal scanning laser ophthalmoscope (SLO) creates an image of the retina by raster-scanning a narrow beam of light across the retina and picking up the reflected light. The confocal technique greatly improves resolution and allows the user to probe tissue at different depths of interest. Longer wavelengths activate different fluorophores and probe deeper layers of the tissue. Compensation for the patient’s eye movements is typically done in post-processing, when the researcher co-registers the images and averages the values for the aligned image stack.
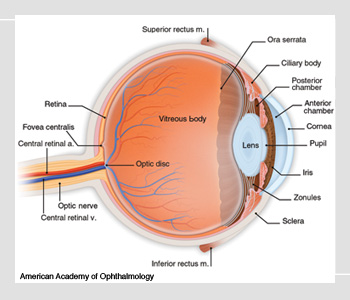 Anatomy of the eye.
Anatomy of the eye.
One of the things that scientists seek to detect with the high resolution of confocal SLO is the apoptosis of retinal cells. Apoptosis is one of the two ways in which cells die. Necrosis refers to the premature death of a cell by acute infection, toxin or trauma. Apoptosis, on the other hand, is controlled by a series of biochemical events. It is a necessary function for multicellular organisms—for example, cell development and selective apoptosis together shape an embryo into a fully formed fetus. “It’s a way the cell commits suicide,” said M. Francesca Cordeiro, professor of retinal neurodegeneration and glaucoma studies at UCL.
However, the process of apoptosis can also be triggered abnormally in glaucoma and other neurodegenerative conditions. Glaucoma affects the optic nerve of the eye, which carries visual information to the brain. It is typically caused by increased pressure on the eyeball that can be related to aging, an eye injury, hereditary factors or other things. Glaucoma can lead to decreased vision, facial pain, eye swelling, sensitivity to light and other problems.
In the past, ophthalmologists have not been able to detect retinal ganglion cells that have died through apoptosis in human eyes, but if they could do so, they could identify glaucoma sufferers before these patients experience vision loss. The earlier glaucoma is caught, the more treatable it is.
Fitzke and Cordeiro have been working on a project called DARC, for Detection of Apoptosing Retinal Cells, for the past six years. The scientists use a fluorescent marker called annexin 5 that identifies cells dying through the process of apoptosis. “You can actually see these cells die in front of you,” she said.
So far, the team has worked with animal models only. In one set of experiments, the UCL researchers induced glaucoma in rats by boosting the intraocular pressure in one eye with a shot of saline solution. They imaged the living eyes with a confocal SLO before and after the injection of the fluorophore, and they checked the amount of apoptosis in retinal ganglion cells several times over a 16-week period. The DARC technique identified apoptosis in 15 percent of cells at peak in a glaucoma model.
Cordeiro and colleagues have hypothesized from their animal glaucoma models that the greatest rate of apoptosis of retinal ganglion cells occurs in the first 10 years of the course of the disease—possibly 10 years before current techniques identify a problem, and an even longer time before the patient starts to notice his or her reduced vision.
Early-phase clinical trials in human glaucoma patients may start as early as this year, Cordeiro said. In the future, this work could also allow physicians to monitor how well they are treating their patients and to assess—with quick turnaround—whether these treatments are working.
Lasers could also play a role in helping researchers to provide an early warning of the onset of Alzheimer’s disease, again by enabling the detection of apoptosis. Amyloid-beta—a peptide that makes up the sticky “plaques” that form inside the brains of people suffering from Alzheimer’s—is also deposited on the retina, where its toxicity causes apoptosis. After all, retinal ganglion cells are nerve tissue too—and thanks to the structure of the eye, these ganglia are much easier to image than the deep regions of the brain. Cordeiro is now studying the connections between glaucoma and Alzheimer’s in the hope of developing new screening tools.
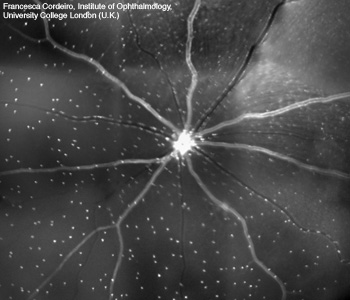 Imaging retinal cell apoptosis. In a recently established technique called DARC (detection of apoptosing retinal cells), apoptosing retinal cells are identified by a fluorescently labeled annexin marker. The image shows the whole retina of a rat that was treated with a retinotoxic agent hours previously. Each white spot is an individual retinal ganglion cell undergoing apoptosis in vivo.
Imaging retinal cell apoptosis. In a recently established technique called DARC (detection of apoptosing retinal cells), apoptosing retinal cells are identified by a fluorescently labeled annexin marker. The image shows the whole retina of a rat that was treated with a retinotoxic agent hours previously. Each white spot is an individual retinal ganglion cell undergoing apoptosis in vivo.
Physicians have been urgently seeking a non-invasive—but accurate—means for diagnosing Alzheimer’s in its earliest stages. A few years back, Lee E. Goldstein of Harvard Medical School (Boston, Mass., U.S.A.) and his colleagues were the first to identify amyloid-beta plaques inside the lenses of the eyes of Alzheimer’s patients (OPN, January 2007, p. 42).
Improving retinal imaging
Scientists are constantly trying to improve SLO technology with adaptive optics and other techniques to increase resolution and image finer details in the structure of the retina.
For example, Alaster J. Meehan, Keith Nugent and colleagues at the University of Melbourne (Australia) recently demonstrated a technique called quantitative phase imaging (QPI), an algorithm for controlling adaptive-optics mirrors in ophthalmoscopes. QPI is a technique that directly calculates the phase of the wavefront by solving the transport of intensity equation. On modern computers, the algorithm runs much faster than the iterative calculation process used by other sensors.
Tested with a 52-actuator mirror in an ophthalmoscope using 655-nm laser light, this alternative method was about as accurate as the familiar Shack-Hartmann wavefront sensor, but it produced better lateral resolution, Meehan said at the recent Frontiers in Optics (FiO) conference in San Jose, Calif. (U.S.A.). The Shack-Hartmann sensor uses a lenslet array to measure the tilt of the incoming wavefront, but its focal length can limit the resolution of a microscopy system.
The optics of the eye limits imaging of the retina, requiring adaptive optics to obtain a diffraction-limited image of that region, Meehan said. With the Shack-Hartmann sensor, the team had difficulty in controlling the actuators around the edge of the mirror. However, with the QPI algorithm, they could use the entire mirror of the microscopy system for higher image resolution and complex beam shaping.
Austin Roorda and colleagues at the University of California at Berkeley (U.S.A.) have studied how to miniaturize the adaptive-optics SLO. These systems have traditionally been large because the adaptive-optics process requires free-space optics; confining the light path to fibers will not preserve the phase. Second, adaptive-optics mirrors were originally designed for larger systems such as telescopes.
The portability and lower cost of smaller systems would promote their clinical use, Roorda said at the recent FiO. The keys to making the SLO more compact are smaller deformable mirrors and good optical design. Instead of using piezo-based deformable mirrors, the team built a system using components based on micro-electro-mechanical systems (MEMS).
Laser eye surgery
Lasers are essential surgical tools for the 21st-century ophthalmologist. With these devices, surgeons can treat a vision-robbing disease such as glaucoma, macular degeneration and diabetic retinopathy. They can also make the patient’s existing vision crisp and clear.
Several laser-based procedures alleviate glaucoma, according to Karen Joos, a clinical and research ophthalmologist at Vanderbilt University in Nashville, Tenn. (U.S.A.). One surgery, called laser iridotomy, treats narrow-angle glaucoma—a severe, acute form of the disease. In this type of glaucoma, the iris of the eye is pushed forward, blocking the channel (angle) that normally allows aqueous fluid to drain. The resulting spike in intraocular pressure causes an acute attack of glaucoma, which may permanently damage the optic nerve.
A risk factor for narrow-angle glaucoma is hyperopia (farsightedness), in which the eye is shorter, front to back, than average. As the crystalline lenses of hyperopic people thicken due to normal aging, they may crowd the small eyes and interfere with the trabecular meshwork of the iris, which normally regulates fluids in the eyeball.
In a laser iridotomy, developed by the French physician Danièle Aron-Rosa about 30 years ago, the ophthalmologist uses an Nd:YAG laser to drill a small hole in the iris to relieve some of the fluid pressure inside the eyeball. Although some types of lasers aid coagulation, the Nd:YAG laser does not, so there is some risk of bleeding in the procedure. For this reason, Joos often starts the surgery by using an argon laser to spur coagulation in the area of the hole and then finishes up with the Nd:YAG laser.
In some cases, the ophthalmologist must perform an iridoplasty with an argon laser and a larger spot size (200 to 400 µm), Joos said. That contracts the iris tissue and cuts a wider hole in it.
Open-angle glaucoma—characterized by a gradual decrease in aqueous fluid outflow despite an open anterior chamber—is a chronic, silent thief of sight. Once the condition has passed beyond the point at which the patient can control it with eyedrops or pills, an ophthalmologist can perform an argon laser trabeculoplasty (ALT), punching 50-µm-size holes in the angle (the region where the cornea and iris meet). According to Joos, it’s believed that the procedure stimulates the tissue to drain the intraocular fluid more effectively.
Within the past five years, researchers have refined this surgery into a technique called selective laser trabeculoplasty (SLT), which uses 532-nm Nd:YAG light with a spot size of roughly 400 µm to increase the drainage in the trabecular mesh. SLT proponents say that it causes less tissue damage to the angle, although some studies have shown that both procedures have equal success rates with patients.
The latest on LASIK
Laser-assisted in situ keratomileusis, or LASIK, is a popular elective surgery with people whose natural vision is worse than 20/20. The procedure for reshaping the cornea to reduce refractive error is now routine in the United States, but researchers have continued to refine the technology incrementally.
Early this decade, wavefront-guided LASIK appeared in the U.S. market. These systems use Shack-Hartmann sensors to measure the original aberrations of the cornea and generate a customized map of the amount of ablation needed to correct the pre-operative refractive error. Wavefront guidance was designed to reduce the amount of glare and haloes that some LASIK patients experience under post-surgical low-light conditions.
Today, the wavefront-guided technology is still considered an upgrade to basic LASIK, but customer demand for it during the current economic recession has been flat, said Jim Schwiegerling, associate professor of ophthalmology at the University of Arizona (U.S.A.). Nevertheless, the technology has expanded the treatment range of LASIK to stronger levels of myopia and astigmatism than what was available in the early days of the surgery. A quarter of the patients who get this procedure can end up with 20/15 or 20/10 vision. With wavefront sensing, people who would otherwise have gotten 20/40 vision after conventional LASIK treatment can now end up with 20/20 vision.
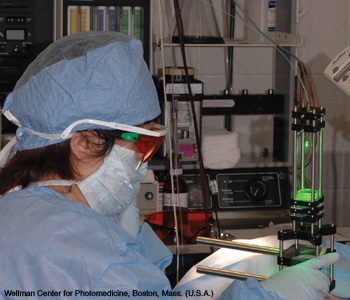 Using a 532-nm laser, surgeon Min Yao performs a photochemical tissue bonding procedure on the damaged cornea of a rabbit. The research could lead to new treatments for humans with corneal damage.
Using a 532-nm laser, surgeon Min Yao performs a photochemical tissue bonding procedure on the damaged cornea of a rabbit. The research could lead to new treatments for humans with corneal damage.
Ultraviolet excimer lasers with an output at 193 nm are the only ones approved for LASIK, according to Schwiegerling. Most ophthalmologists use narrow-beam LASIK systems, with spot sizes of 1 to 2 mm, instead of the early broad-beam systems with mechanical apertures.
The manufacturers of LASIK lasers have also made them easier to use by adding eye tracking to the laser. Since the patient is conscious during the procedure, some small eye movements are inevitable. Previously, the surgeon would use a joystick to keep the instrument centered on the eye. However, most modern systems use video-based eye tracking to follow features on the iris to calculate where to deliver the laser power. Usually the patient’s eye motions are pretty small—less than 0.5 mm in any direction—but the surgeon must take out a precise amount of tissue in order to avoid introducing higher-order aberrations such as spherical aberration and coma.
Femtosecond lasers, operating in the near-infrared, have begun to play a different role in LASIK surgery: Cutting the flap in the cornea so that the surgeon can use the excimer laser to reshape the inside of the cornea.
In the original LASIK procedure, the surgeon would use a mechanical oscillating-blade device called a microkeratome to cut a flap 100 to 200 µm thick in the cornea, which is about 500 to 600 µm thick. Now, the surgeon flattens the cornea with a small plate, and then the femtosecond laser pushes infrared energy into the cornea. The bursts of energy create small cavitation bubbles about 150 µm from the surface of the cornea. Once the ophthalmologist has created enough of those bubbles, the tissues can be separated into a flap.
The bubble-flap technique is still considered a premium service, but about half of all LASIK patients are now choosing it, according to Schwiegerling. People prefer the laser to the microkeratome because the former “has the feeling of being much more benign than the razor blade,” he said.
Surgery to install intraocular lenses (IOLs) to replace cataract-clouded natural lenses is still a mechanical procedure, but laser treatment can rectify one of its complications. Some post-surgical cataract patients develop a translucent film that grows on the back of the IOL. This process is called posterior capsule opacification. The surgeon can use an Nd:YAG laser to dissolve some of that film and open an aperture for improved vision, Schwiegerling said.
Fixing damaged corneas
Sometimes ophthalmic surgeons need to repair corneas damaged by burns, acids, accidents or other trauma. Conventionally, they use sutures to attach transparent slices of sterilized human amniotic membrane—roughly 30 µm thick—to the damaged corneal tissue. However, inflammation and scarring are frequent side effects of the surgery.
Plastic surgeon Min Yao and colleagues at the Wellman Center for Photomedicine (Massachusetts General Hospital and Harvard Medical School, U.S.A.) have developed a laser-based technique that could reduce these complications. The team has performed the technique only on rabbits so far, but the early results are promising.
Yao adapted a procedure that plastic surgeons already use to close some small skin wounds. It’s called photochemical tissue bonding (PTB), and it uses a well-known stain called rose bengal that already has multiple medical uses.
In the PTB procedure, the surgeon stains the thin slice of amniotic membrane, which has been harvested from the innermost layer of the human placenta, with the rose bengal solution. Then the physician places the tissue on the injured cornea and irradiates it with a 532-nm Nd:YAG laser with a doughnut-shaped beam (a black contact lens over the eye’s pupil guards against retinal damage). According to Yao, the rose bengal absorbs the green light, which locally heats the collagen in both kinds of tissue and causes the proteins to bond with each other via the intertwining and mixing of the collagen fibrils.
In comparing PTB and conventional surgical procedures, Yao found that the PTB-treated eyes had less scarring, inflammation and neovascularization (growth of new blood vessels) than
the sutured eyes. After all, sutures actually cause tiny new injuries to the delicate corneas.
“With bonding, we don’t cause any additional injury,” she said. In addition, the PTB procedure takes less than five minutes to complete, whereas suturing the rabbit eye takes at least 20 minutes.
Yao hopes that clinical trials of PTB can take begin two years from now, but she and her Wellman colleagues, including biochemist Irene Kochevar, are still designing the protocols for human experiments. Avoiding damage to the retina during the procedure will be a major concern for the team.
Looking forward
Many research teams around the world are vigorously pursuing higher-resolution retinal imaging using AO, optical coherence tomography (OCT) and lasers with exotic optics. Improved surgical techniques with lasers could result in faster healing and less scarring.
The imaging and surgical research going on today could have profound implications for tomorrow’s patients, who will enjoy clear, comfortable vision for many more years than was previously possible.
Patricia Daukantas is the senior writer/editor of Optics & Photonics News.
Extended List of References and Resources
>> O. Callender. "Diagnosing Glaucoma with Laser Precision," Opt. Photon. News 15(5), 22 (May 2004).
>> J. Carroll et al. "Recent Advances in Retinal Imaging with Adaptive Optics," Opt. Photon. News 16(1), 36 (January 2005).
>> A.V. Cideciyan et al. "Reduced-illuminance autofluorescence imaging in ABCA4-associated retinal degenerations," J. Opt. Soc. Am. A 24, 1457 (2007).
>> M.F. Cordeiro et al. "Real-time imaging of single nerve cell apoptosis in retinal neurodegeneration," Proc. Natl. Acad. Sci. USA 101, 13352 (2004).
>> A.E. Elsner et al. "Imaging in the Aging Eye," Opt. Photon. News 11(7), 20 (July 2000).
>> J.J. Ewing. "Excimer Lasers at 30 Years," Opt. Photon. News 14(5), 26 (May 2003).
>> A.V. Goncharov et al. "Laboratory MCAO test-bed for developing wavefront sensing concepts," Opt. Express 13, 5580 (2005).
>> A. Greenaway. "Adaptive Optics: Astronomy and Beyond," Opt. Photon. News 17(9), 22 (September 2006).
>> L. Guo et al. "Targeting amyloid-β in glaucoma treatment," Proc. Natl. Acad. Sci. USA 104, 13444 (2007).
>> J. Hunter et al. "Unexpected Retinal Damage Below the ANSI Standard," in Frontiers in Optics, OSA Technical Digest (Optical Society of America, 2009), paper FTuQ2.
>> T. Juhasz et al. "The Femtosecond Blade: Applications in Corneal Surgery," Opt. Photon. News 13(1), 24 (January 2002).
>> S. Marcos. "Refractive Surgery and Optical Aberrations," Opt. Photon. News 12(1), 22 (January 2001).
>> A.J. Meehan et al. "High Resolution Wavefront Sensing and Mirror Control for Vision Science by Quantitative Phase Imaging," in Frontiers in Optics, OSA Technical Digest (Optical Society of America, 2009), paper JWB5.
>> G.M. Morris and L.T. Nordan. "Phakic Intraocular Lenses: The New Focus in Refractive Surgery," Opt. Photon. News 15(9), 26 (September 2004).
>> G. Popescu. "Quantitative phase imaging: taking the pulse of living cells," SPIE Newsroom, doi: 10.1117/2.1200702.0710 (February 4, 2007).
>> H. Rashed et al. "Optical Coherence Tomography of the Retina," Opt. Photon. News 13(4), 48 (April 2002).
>> A. Roorda et al. "Miniaturization of Adaptive Optics Scanning Laser Ophthalmoscope," in Frontiers in Optics, OSA Technical Digest (Optical Society of America, 2009), paper FWX1.
>> S. Schmitz-Valckenberg et al. "Real-Time In Vivo Imaging of Retinal Cell Apoptosis after Laser Exposure," Invest. Ophthalmol. Visual Sci. 49, 2773 (2008).
>> J. Schwiegerling. "LASIK and Beyond," Opt. Photon. News 13(1), 30 (January 2002).
>> J. Schwiegerling. "Wavefront-Guided LASIK," Opt. Photon. News 15(2), 26 (February 2004).
Additional Resources
Links to organizations related to lasers in ophthalmology are as follows:
American Academy of Ophthalmology
American Society for Laser Medicine and Surgery
American Society of Cataract and Refractive Surgery
Asia Pacific Academy of Ophthalmology
Association for Research in Vision and Ophthalmology
European Society of Cataract and Refractive Surgeons
Eye Surgery Education Council
International Commission on Non-Ionizing Radiation Protection
International Council of Ophthalmology
International Society of Refractive Surgery
National Eye Institute (U.S.A.)
World Ophthalmology Congress 2010 (June 5-9, Berlin, Germany)

