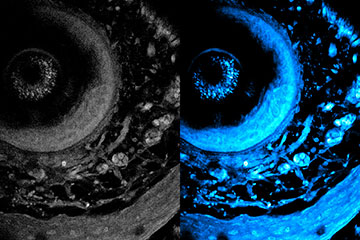
The new technique enables laser light to penetrate deeper into living tissue. On left is the initial image, and on right is the optimized image using the new technique. [Image: Courtesy of Sixian You et. al.]
Researchers at the Massachusetts Institute of Technology (MIT), USA, have developed a new optical imaging technique that they say allows for nondestructive, high-resolution visualization of deeper biological tissues than previous systems (Sci. Adv., doi: 10.1126/sciadv.adp2438). The label-free method, a variation on two-photon autofluorescence imaging, can penetrate to more than 700 μm into living human tissue samples—more than double the usual depth limit of metabolic imaging. The results represent an advance for deep imaging of intact living biological systems for applications like cancer research, immune responses and tissue engineering.
Improving metabolic imaging
Optical metabolic imaging has been increasingly employed in biomedical research to understand disease pathology and predict treatment response. For example, two-photon autofluorescence imaging of endogenous fluorophores, such as reduced form nicotinamide adenine dinucleotide phosphate [NAD(P)H], does not require labeling agents that may perturb the natural biological processes, dynamics and response of live cells or tissues.
However, NAD(P)H imaging has been restricted to superficial tissues, as the depth limit rarely extends beyond 300 μm due to light scattering and other factors. Sixian You and her colleagues at MIT propose a new approach, which they call deep and dynamic simultaneous label-free autofluorescence-multiharmonic (dSLAM) microscopy, in which they adaptively customize the laser light for deep tissues.
“This work shows a significant improvement in terms of depth penetration for label-free metabolic imaging,” said study author You, in a press release accompanying the research. “It opens new avenues for studying and exploring metabolic dynamics deep in living biosystems.”
Testing its capabilities
The researchers leveraged three-photon excitation of NAD(P)H to substantially reduce scattering and enhance the signal-to-background ratio in deeper tissues. They achieved high peak power that exceeded 0.5 MW at 1100 nm with a multimode fiber coupled to a compact fiber shaper, which allowed them to precisely modulate the light propagation by adaptively changing the shape of the fiber.
The deep 3D-imaging capability enabled noninvasive visualization of the complex multicellular interactions, metabolic states and depth-dependent variations within the model.
To test the dSLAM microscope, You and her colleagues acquired living blood–brain barrier microfluidic models with different cell types. The deep 3D-imaging capability enabled noninvasive visualization of the complex multicellular interactions, metabolic states and depth-dependent variations within the model. To examine its capability for capturing faster dynamics, they also employed dSLAM to track the metabolic activities and motility features of 50 white blood cells in vitro over a 150-second imaging session.
“To move toward clinical translation, we aim to further extend the depth and maintain the multimodal metabolic contrast while minimizing photodamage,” You said.
