![]()
A team at USC has developed an OCT-enabled otoscope that it says could provide considerably more information than the conventional version pictured here. [Image: The Good Brigade / Getty Images]
Most people know the experience well: In the course of a routine physical examination, the doctor takes a quick look at the patient’s eardrum, or tympanic membrane (TM), tickling the ear canal with a simple examining tool called an otoscope. Unfortunately, the common doctor’s-office otoscope—often essentially a combination of a light and a lens—can provide a view only of the eardrum’s surface. And even that can be obscured if the patient is suffering from certain ear diseases.
Now, a research team headed up by Brian Applegate at the University of Southern California (USC), USA, has put optical coherence tomography (OCT) on the case, developing an otoscope designed to look wider and deeper (J. Biomed. Opt., doi: 10.1117/1.JBO.29.8.086005). In clinical experiments, the team’s handheld OCT device—a new iteration on a device unveiled three years ago (Biomed. Opt. Express, doi: 10.1364/BOE.430935)—reportedly can image the 3D structure of the TM, as well as glimpse beneath the eardrum into the structures of the middle ear. The researchers believe their otoscope “can readily fit into the hearing clinic workflow and provide new relevant information for diagnosing and managing TM and ME disease.”
From eye to ear
OCT, an interferometry-based tool, provides a clinical picture analogous to the one from ultrasound, in which a 2D cross-sectional picture is successively built up from echoes off of layers at depth. In OCT, however, the “echoes” are echoes of light delivered by an ultrafast laser, enabling the delineation of features at a far finer scale. Originally developed in the 1980s for imaging of the retina, the technique has since then revolutionized optical examinations, and has expanded into a range of other uses in medicine, industry and even art conservation.
Efforts of researchers to put OCT to work in imaging the TM and middle ear date back to the early 2000s. Much of the action since then has attempted to push toward a device sufficiently small, flexible and easily handled for routine clinical use. In its 2021 study, the USC team behind the new work introduced such a handheld OCT otoscope and tried it out in nonclinical tests on several volunteers. The team’s new study has now introduced a few mods to get the device closer to a practical clinical implementation, and demonstrated its ear-imaging chops in trials on scores of patients at a hearing clinic.
OCT + video
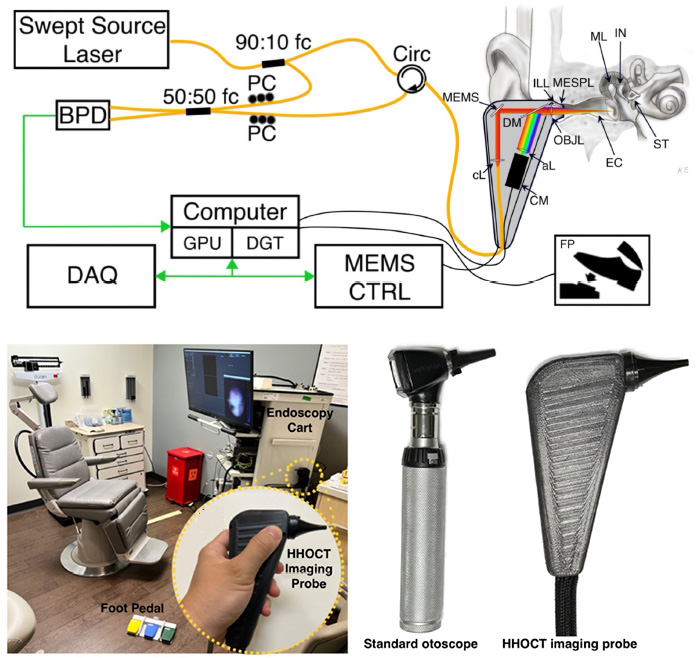
Top: A schematic of the OCT otoscope. 90:10 fc, 90:10 fiber fused coupler; Circ, fiber optic circulator; cL, collimating lens; MEMS, MEMS scan mirror; DM, dichroic mirror; ILL, illuminator; OBJL, objective lens; MESPL, middle ear speculum; EC, ear canal; ML, malleus; IN, incus; ST, stapes; aL, achromatic lens; CM, video camera; PC, polarization controller; 50:50 fc, 50:50 fiber fused coupler; BPD, balanced photo-detector; GPU, graphic processing unit; DGT, digitizer; DAQ, data acquisition board, MEMS CTRL, MEMS scan mirror controller; FP, foot pedal. Bottom left: Clinical setup. Bottom right: Handheld OCT device compared with a conventional otoscope. [Image: W. Kim et al., J. Biomed. Opt. 29, 086005 (2024), doi: 10.1364/BOE.430935; CC-BY 4.0
The device showcased in the new paper begins with a custom-built swept-source laser chip from Insight Photonics Solutions, Inc., the output from which is split, with 90% of the energy sent into the interferometer sample arm (the imaging device) and 10% into the reference arm. The back-reflected light from the device is combined with the reference-arm light and sent to a balanced photodetector, the signal from which subsequently is routed to a computer for processing.
In addition to the OCT light, the otoscope captures reflected RGB light on a CMOS sensor and sends it directly to the computer, enabling a standard video otoscope image to complement the OCT imaging. The electronics to control the handheld device fit on a rollable endoscopy cart, with the firing of the handheld device controlled by the clinician using a foot pedal.
The OCT otoscope sports a lateral resolution of 38 µm and an axial resolution of 33.4 µm. The researchers tweaked the optics from their 2021 design to enable a much wider field-of-view (FOV) of 7.4-mm diameter. And they topped things off with a computer algorithm to compensate for possible aberrations due to the larger FOV.
Peering into ear pathologies
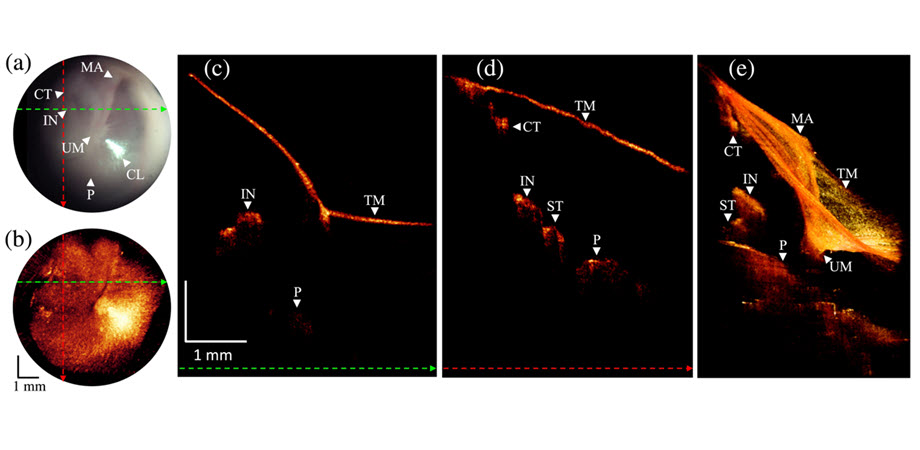
The researchers tested out the latest iteration of their OCT otoscope in a clinical study involving 100 patients at the hearing clinic of the USC Keck Hospital. The team found that the instrument was able both to provide more detailed imaging of healthy eardrums, and to unveil a number of subtle pathologies and clinical signs that are harder to suss out with conventional otoscopy. These include some forms of inflammation of the TM; monitoring the healing process of perforated eardrums; “retraction pockets” in the TM and air pockets in the middle ear; and other examples.
Imaging of a normal/healthy ear using the OCT otoscope. (a) and (b): Comparison of visuual otoscope (top) and OCT (bottom) image. (c and d) B-scan OCT cross sections corresponding to green and red dashed lines in (a) and (b). (e) 3D volume rendering. MA, malleus; CT, chorda tympani; TM, tympanic membrane; IN, incus; UM, umbo; CL, cone of light; P, promontory. [Image: W. Kim et al., J. Biomed. Opt. 29, 086005 (2024), doi: 10.1364/BOE.430935; CC-BY 4.0
According to the USC team, operating its OCT otoscope is “sufficiently easy” that “a single person can collect a set of images from a patient in seconds to minutes,” allowing the Keck Hospital trial to take place “without disrupting the workflow within the clinic.” The team believes its findings “further demonstrate hand-held OCT’s ability to be a useful clinical tool” in the realm of ear health and hearing disorders.